Does Telepractice Benefit Everyone?
Factors That Determine Candidacy for Telepractice
Ramachandar, S., Ph.D1 , Parfitt, M., MA, LSLS Cert. AVEd2, and Moncrieff, D., Ph.D3 Southern Connecticut State University1, DePaul School for Hearing & Speech2, University of Memphis3
PURPOSE OF THE STUDY
To identify factors that are related to positive outcomes in therapy delivered through a telepractice platform
BACKGROUND AND RATIONALE
- Telepractice can be an effective method to offer parent education to families who have limited access to qualified professionals.
- A number of factors including time constraints, issues with technology and inherent child features can influence the success of the therapy provided through telepractice.
- When considering a telepractice option for a client it would be beneficial for clinicians to know which factors consistently resulted in positive outcomes for students and which factors were often indicators of limited success.
- This is a follow-up analysis of data obtained from our study investigating the efficacy of parent education via telepractice in listening and spoken language skills of children with hearing loss.
METHODS
- 27 families of children with hearing loss between the ages of 2 and 7 years were recruited for the original study.
- 16 Families received telepractice sessions (5 families completed the study)
- 11 families in face-to-face group (6 completed the study)
- Sessions were conducted once per week for 45-60 minutes by a licensed SLP under the supervision of a Listening & Spoken Language Specialist.
- Services were provided for approximately 9 months.
- Pre and post intervention measures included:
- Standardized language testing of child
- Video of parent child interaction with observable parent skills rating by clinician
- Parent completion of a self-report questionnaire
SUMMARY
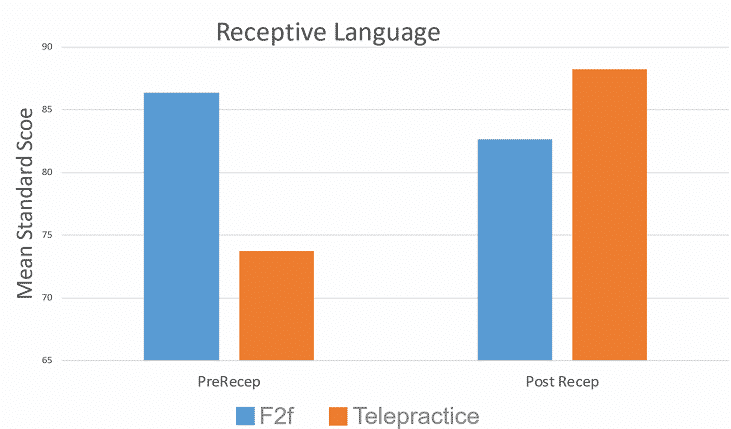
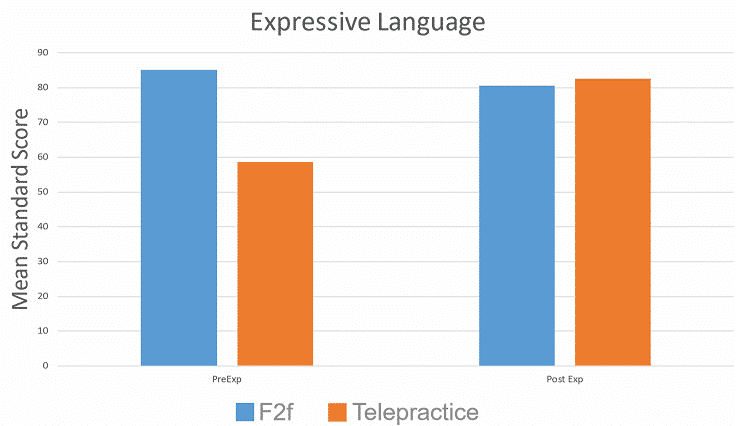
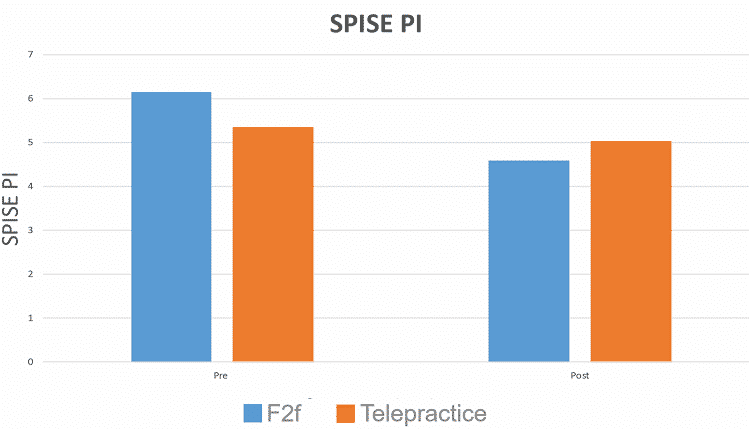
- No statistical difference between post language scores between groups.
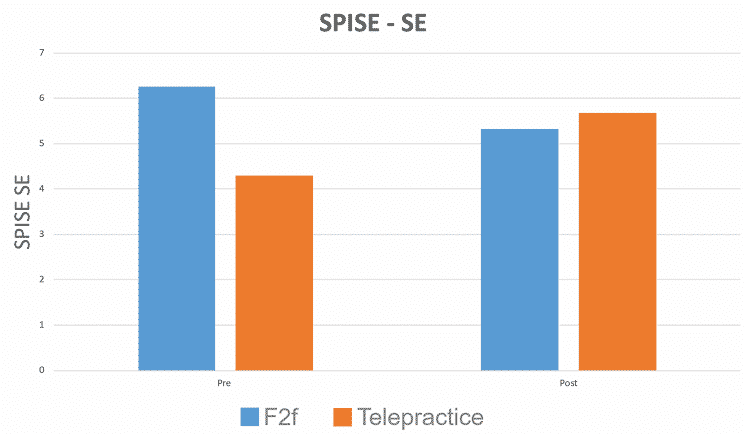
- No statistical difference between between post SPISE: Self-Efficacy and Parental Involvement scores between groups.
FACTORS THAT HINDERED SUCCESSFUL TELEPRACTICE OUTCOMES
(in order of impact degree)
- Technical difficulties
- Family factors (i.e. Both parents working, Siblings, Relocation, Motivation Commitment to facilitating spoken language, Presence of additional speech services)
- Child factors (i.e. Attention)
RESULTS
REFERENCES
Crutchley, S., & Campbell, M. (2010). TeleSpeech therapy pilot project: Stakeholder satisfaction. International Journal of Telerehabilitation, 2(1), 23.
Lincoln, M., Hines, M., Fairweather, C., Ramsden, R., & Martinovich, J. (2014). Multiple stakeholder perspectives on teletherapy delivery of speech pathology services in rural schools: A preliminary, qualitative investigation. International Journal of Telerehabilitation, 6(2), 65.
Percy-Smith, L., Jensen, J. H., Cayé-Thomasen, P., Thomsen, J., Gudman, M., & Lopez, A. G. (2008). Factors that affect the social well-being of children with cochlear implants. Cochlear Implants International, 9(4), 199–214.
Reynolds, A. L., Vick, J. L., & Haak, N. J. (2009). Telehealth applications in speech-language pathology: a modified narrative review. Journal of Telemedicine and Telecare, 15(6), 310–316. https://doi.org/10.1258/jtt.2009.081215
Telepractice: Overview. (n.d.). Retrieved April 4, 2019, from American Speech-Language-Hearing Association website: https://www.asha.org/Practice-Portal/ Professional-Issues/Telepractice/
Watkin, P., McCann, D., Law, C., Mullee, M., Petrou, S., Stevenson, J., … Kennedy, C. (2007). Language ability in children with permanent hearing impairment: the influence of early management and family participation. Pediatrics, 120(3), e694–e701.
Forducey, P., Speech telepractice program expands options for rural Oklahoma schools. The ASHA Leader, 2006.11(10): p.12-13.
Grogan-Johnson, S., et al., A pilot study comparing the effectiveness of speech language therapy provided by telemedicine with conventional on-site therapy. Journal of Telemedicine and Telecare, 2010. 16(3): p. 134-139.
Waite, M.C., et al., A pilot study of online assessment of childhood speech disorders. Journal of Telemedicine and Telecare, 2006. 12(Suppl 3): p. 92-94.
Cason, J., A pilot telerehabilitation program: Delivering early intervention services to rural families. International Journal of Telerehabilitation, 2009. 1(1): p. 29-38.
Kelso, G.L., et al., The Feasibility of Virtual Home Visits to Provide Early Intervention: A Pilot Study. Infants and Young Children, 2009. 22(4): p. 332-340.
Behl, D.D., et al., Tele-Intervention: the wave of the future fits families’ lives today, 2010, EP Global Communications, Inc. p. 22.